Dear ARBDA Community,
The Entire Team at Arthritis, Rheumatic, & Back Disease Associates wants you to be aware of steps that we’re taking to ensure your safety in our offices as well as provide some general guidance to address a number of the questions/concerns we’ve received regarding the COVID-19 virus.
Your ARBDA Physicians are continuously monitoring the Centers for Disease Control (CDC), World Health Organization (WHO), and other public health institution(s) information to review any updated information & adapt our protocols (if necessary). Our Physician & Administrative Teams lead our efforts to ensure that all ARBDA locations continue to serve the community at the same level of care you have come to expect from us, especially during this time of uncertainty. To that end, some of the steps that we’re taking to ensure the safety of our patients & staff members include: drastically increasing the frequency and duration of our disinfection protocols, providing staff & patient education on proper respiratory hygiene and hand washing techniques, and identifying patients who may be at high risk of contracting the illness caused by the COVID-19 virus to prevent any possible transmission (among many others).
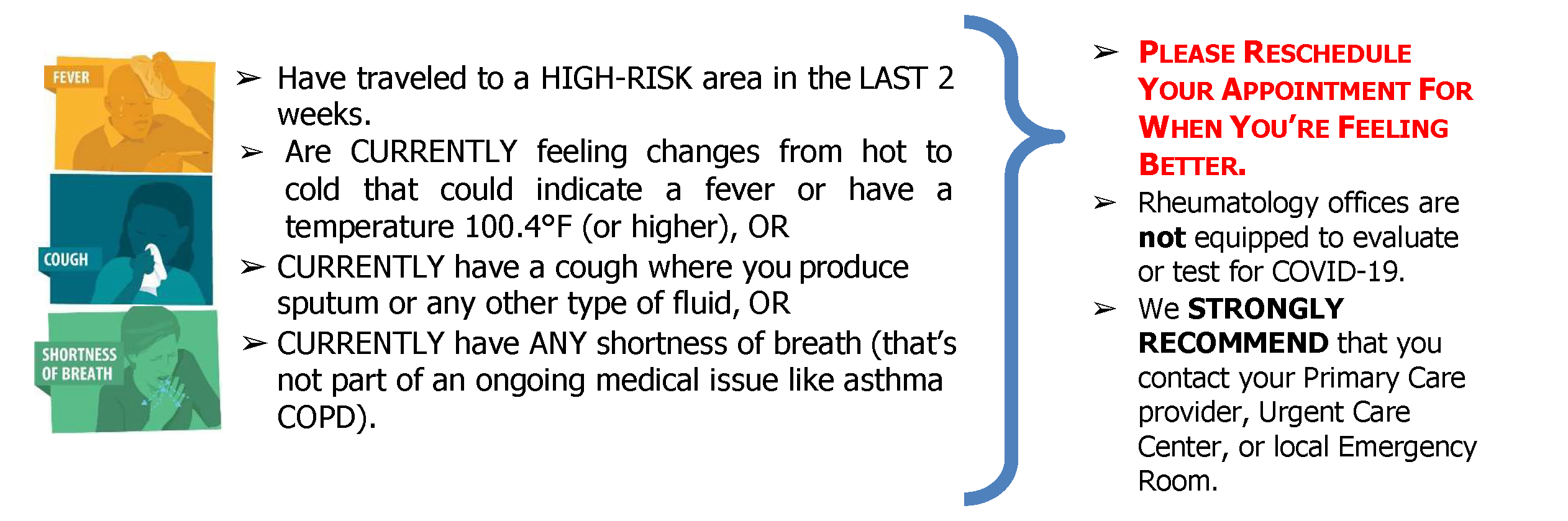
However, all of those efforts would be incomplete if we did not also ask for your help. If you are scheduled for an appointment or infusion AND answer YES to ANY of the following:
We’re often asked the following questions and hope that these general guidelines will be helpful for you – including those that relate to medicines which we may prescribe to you.
BASIC PRECAUTIONS: Reducing the spread of respiratory illness is the biggest step that anyone can take to combat infections. By helping to do your part in reducing the spread of COVID-19 and other illnesses – you ensure that your fellow ARBDA patients are less likely to suffer the effects of infection.

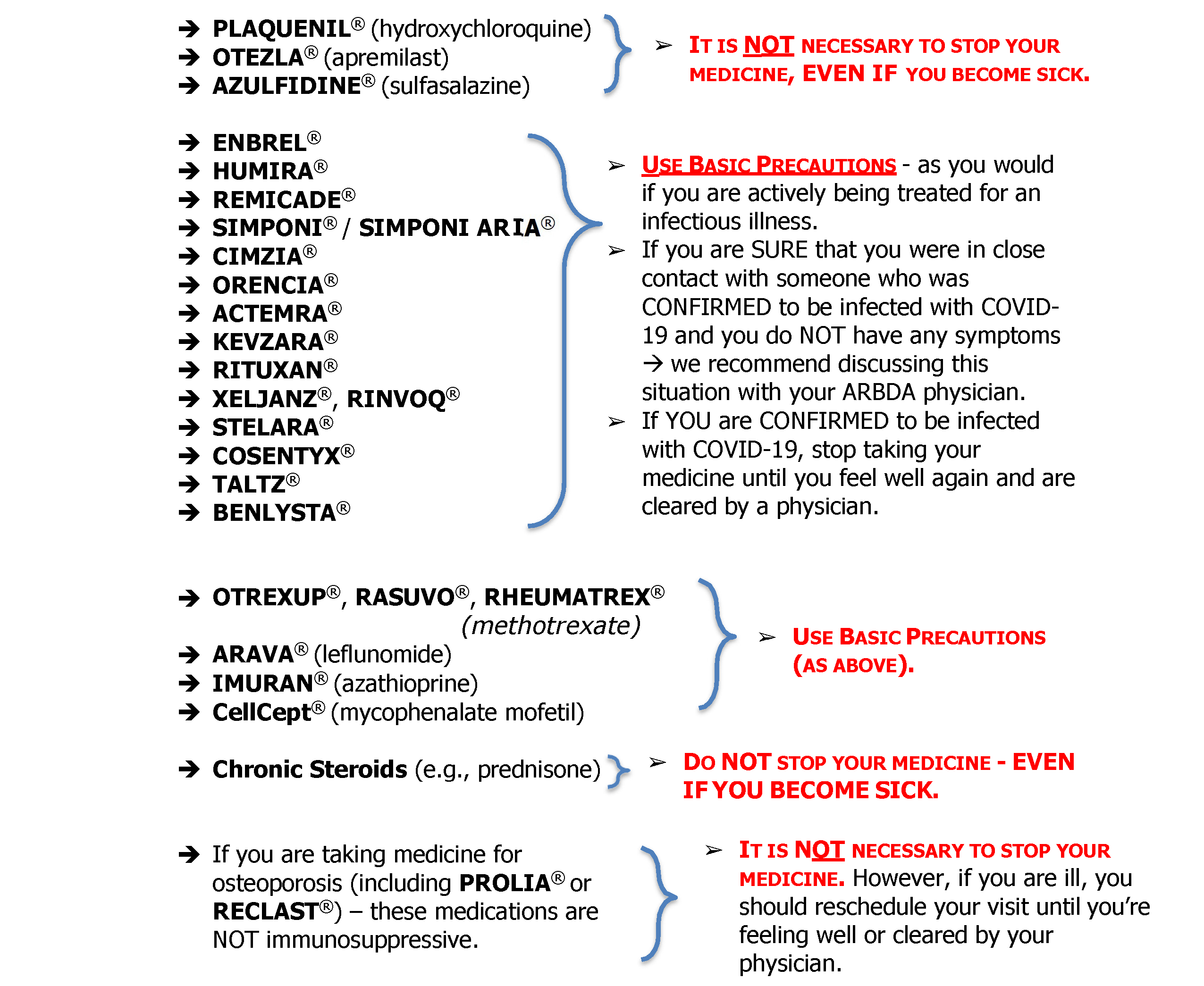
GUIDANCE FOR PRESCRIBED MEDICATIONS
** NOTE ** Please consult with your ARBDA physician PRIOR to stopping any treatment. The following guidance generally applies for patients currently taking:
Other Frequently Asked Questions
1. Can COVID-19 be prevented?
There are measures that you can take to reduce the chances. Please see Page 2 for instructions. Experts do NOT recommend wearing face masks UNLESS YOU ARE SICK or caring for someone who has (or might have) COVID-19.
2. How is COVID-19 treated?
Unfortunately, there are no currently approved vaccines to prevent COVID-19 infection nor approved treatments for those that are currently infected. Therefore – treatment is really targeted to relieving symptoms and providing the body with the support that it might need to fight any other infection. There are currently a few different treatments which are being tested for use – but none have completed clinical trials at this point.
3. Do patients known to be infected with COVID-19 need to be hospitalized?
As with all infectious diseases, whether a person needs to be hospitalized or not largely depends on their particular symptomatic presentation and disease course. So, put simply, unless a particular patient has (or develops) moderate to severe symptoms – they likely do not need to be hospitalized. However, all patients should follow the guidance of their primary care and/or urgent care physicians with respect to treatment and ongoing care for COVID-19.
4. Can people who recover from COVID-19 be infected again?
The complete immune response to COVID-19 infection is not completely understood as of yet. In similar viruses, patients are less likely to be reinfected shortly after recovery. However, at this point in time, the science is still evolving on this topic.
5. When is someone infectious?
Generally, the incubation time for COVID-19 is between 2-14 days. In patients who had family members who were infected – their symptoms generally appeared within 3-6 days. However, the 14-day time period appears to be the standard at this point in time until we know more about the evolution of this particular virus.
6. Which body fluids can spread infection?
Generally, as gross as it may sound, any bodily fluid that is wet is likely to spread the infection. This is why hand washing and surface disinfection are VERY IMPORTANT. Droplets of saliva or respiratory excretions can spread 6-9 feet when someone coughs. Covering your mouth and coughing into a tissue is the best way to reduce transmission (followed by washing your hands for a MINIMUM of 20 seconds).
7. I am currently prescribed an immunosuppressive medication – should I work from home?
The accepted standard of care for patients currently prescribed immunosuppressive medications is that any type of self-quarantine or selfisolation is NOT necessary unless there is known contact with a confirmed infectious patient, an individual patient is experiencing symptoms, and/or the local Department of Health recommends such measures to reduce community-wide spread of an infectious disease.
That said, patients should keep in mind that due to the evolving nature of the current situation – such recommendations may change quickly and without much notice.
If you have additional questions or concerns, please contact your ARBDA physician to arrange a phone consultation
** NOTE ** Due to the rapidly changing pattern of the current epidemic, these guidelines are meant simply as general information. We will attempt to provide updates as new information becomes available. However, given that the basic science involved in understanding the immune response to COVID-19 is rapidly changing – this information may change frequently, without notification, and is not meant to replace/supersede the advice of your Rheumatologist.
** Most Recent Update: 13 March 2020 at 1158am